It’s been just over a hundred years since women gained the right to vote and to enter parliament, back in 1918. But, has anything really changed? On the surface, some would argue that gender equality is on the horizon and the tide is turning. The rest of us, however, are under no illusions regarding the situation we currently find ourselves in.
With April fast approaching, the new corporate gender pay gap report will soon be accessible nationwide. Comparatively, at this point, it seems that the gap has slowly begun to close, but it’s important to remember that 62% of those who are earning less than the living wage are – you guessed it – women. What is particularly mystifying about the pay gap, is the disparity between the sexes and their representation in educational institutions. Women make up 76.1% of students in higher education, but corporate boardrooms and real positions of power are still continuously monopolised by men – who make up nearly 75% of these types of roles. We see an almost inverse of numbers between higher educational participants, and those who actually dominate across all industries. It’s not just office politics and meeting rooms that are entrenched in patriarchy. Nothing is safe… not even the air conditioning. Boris Kingma conducted a study that iterated that most air conditioning temperatures are still based on a 1960 model – that was specifically tailored to the metabolic rate of a 70 kg, 40-year-old white man. Women find themselves on the back-foot, as our rates are an average of 3 degrees higher than most men.
And it doesn’t stop there. Workplace disparities make up one part of the problem. The other exists within the household – even retreating to the comfort of their own homes does not keep misogyny at bay. ONS data analysis suggests that women carry out more unpaid work than men, with an overall average of 60%. The idea that women should be confined to the home, where they are dutiful wives and mothers is prevalent across the board, as unpaid work is consistent among every age group surveyed. From those classed as underage at 25, to those in the older category, age 56 and over.
This blatant inequality between the sexes is felt by women from all walks of life. It’s enough to drive any of us insane. But I’d wait before running to the doctor. That isn’t a safe space either as, ‘the interaction between patriarchy and women’s health […] [is] well-reported’. It seems that nowhere is safe from the confines of oppression, belligerent attitudes, or misplaced intentions where women are concerned. Even as we’ve seen a rise in womanism, and intersectional feminism in the 21st century, it seems that it really is a man’s world after all. For those who are in denial, I want to dig a little deeper into the inherent medical bias towards women that is present within our current, global healthcare system.
The Perception of How Women Deal With Pain
Women are biological powerhouses. We menstruate each month, carry and birth children – pushing another human being out of our bodies. Not that the medical system cares, really. Stereotypically, women are seen as the weaker of the sexes, more susceptible to pain, and more likely to see the doctor for more trivial symptoms. Interestingly though, none of this is supported by any actual evidence. Every study that has been conducted in line with the above attitudes has highlighted that there is no truth to those claims, at least not scientifically. Bearing that in mind, how did we get here? Where have these ideas come from? Society.
Let’s look at this through a historical and intersectional lens – generally, the mainstream ways of thinking are centred around whiteness and patriarchy. White men, especially, are portrayed as brave, strong and true; whilst brown and black men are marketed as dangerous, sexually aggressive and a threat to both white virility and the established status quo. White women offer a picture of innocence, chastity and helplessness; brown and black women are either subservient/angry (the tropes differ across these groups of women), over-sexual and animalistic. Is it any wonder why women are ignored or mistreated within healthcare given the narratives that are pushed upon us in society? It’s interesting to note that there is also a medical disparity among women, as women of colour do not receive the same treatment afforded to their white counterparts (we will get to that issue later – watch this space).
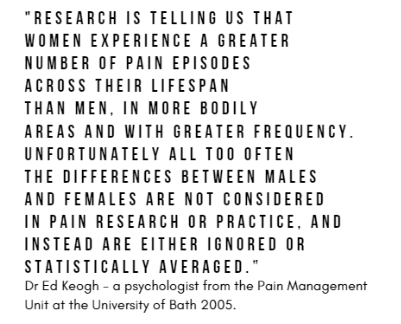
Medically, studies have concluded that women deal with more pain, and experience it more often across our lifetimes. This information is actually 14 years old, and a credit to the University of Bath – but I have to ask how widely held this knowledge actually is. If we know that women are in more chronic pain, more often, and feel that pain more intensely… why is this pain still not believed or held in high regard by the medical professionals that treat us?
I think if anything this serves as a critique of the inherent bias that we have allowed to infect our current medical systems – and this is strengthened when we examine another study. Generally, it’s assumed that women visit the doctor more regularly than men, for more trivial issues. A UK study disproved this when they concluded that the evidence to support these claims were ‘surprisingly weak and inconsistent’. This is where the battle of gender disparities in healthcare begins. Not only are we going to have to fight tooth and nail for advocacy, funding, research, support – but also to unsettle the preconceptions and fairy tales that exist around women and our bodies.
The Struggle to be Heard, Diagnosed or Referred
I know this particular struggle personally. I’ve been diagnosed with Endometriosis, Polycystic Ovarian Syndrome and Adenomyosis for just over a year now. These are all notoriously difficult conditions to diagnose. On average, it can take 8-10 years alone to diagnose Endometriosis in the UK. Even though as a condition, it is gaining more media attention and awareness every day, it is still something that’s systematically ignored by healthcare professionals. Standardisation around diagnosis and treatment has been implemented within the NHS, it is still not followed as it should be. Why does it take so long to diagnose a condition that is affecting 10% of all women within the UK? The answer is probably obvious to some. Women are systematically ignored by their doctors, are not asked any questions that would highlight or pinpoint obvious symptoms, and there is a sense of lingering hysteria within the current medical system. This stems from the idea of female hysteria within Western medicine, in the 1950s – any woman who displayed a desire for sexual activity was seen to be suffering from the disease. Doctors would treat this condition by the way of a pelvic massage, which was laborious… giving rise to the vibrator. Contemporary medics have debated the subject and found that the symptoms of hysteria are ‘synonymous with normal functioning female sexuality’. Although women are not regarded in the exact same way now, there is still the impression that female hysteria plays a part within the doctor’s office.
Any woman that’s suffered from a chronic condition, specifically reproductive health has probably heard one or all of the following phrases:
‘the pain can’t be that bad, you’re overexaggerating’
‘this is normal for you and your body’
‘it will settle down when you have a child or fall pregnant’ – there are instances where this is told to teenagers suffering from endometriosis
‘maybe you should lose some weight’
I wonder if men are afforded the same treatment when it comes to medical professionals. Statistically, it seems not, actually. Whilst women are categorised as psychiatric patients and given anxiety medication, men are comparatively given higher dosages of medication and tests to rule out medical conditions. J.Crook and E. Tunks conducted a study ‘Women with Pain’ that deduced “women with chronic pain conditions are more likely to be wrongly diagnosed with mental health conditions than men and prescribed psychotropic drugs, as doctors dismiss their symptoms as hysterics”.
Not only that, when women and men both presented the exact same symptoms and levels of abdominal pain – research found that they are more likely longer to wait at A&E. Men were asked to wait for 49 minutes to be seen, whilst women were only seen after 65. Given that we statistically and medically, bear more pain, and experience more of it; why are women yet again on the back-foot when it comes to medical treatment? This phenomenon is not specific to one place in the world, either. It operates on a global scale.
In 2016, the United States ran a study concerning gender bias within emergency room settings, by analysing a database containing every heart attack case, from every ER in the country. The results were not unexpected, but in some ways, are shocking. The study concluded that a heart attack patient is more likely to die if they are a female, being treated by a male as opposed to a same-sex doctor-patient relationship. They recorded the figure at 12%. This means that 1 out of 66 women dies within that context when they are not treated by another woman. Don’t these kinds of studies actively challenge the notion that doctors should and will ‘do no harm’ and not allow biases to cloud their judgement or ability to empathise with a patient?
Lack of Female Presence in Clinical and Pre-Clinical Trials
Being heard is not just an issue that is prevalent in emergency rooms, it is the basis of healthcare itself that worries me the most. In her book, Pain and Prejudice, Gabrielle Jackson explores the lack of female test subjects within medical trials and tests. Although this has increased since the 90s, researchers still do not always analyse the results in line with the different sexes. When knowing the inherent differences in our bodies, biological composition and responses to pain – how is this still medically or scientifically sound in the 21st century? Clinical studies may have changed, but pre-clinical studies ‘remain focused on male cell lines and male animals. In 2010, Annaliese Beery and Irving Zucker reviewed how our gender bias has seeped into research on mammals and their historical precedents. “Male bias was evident in eight disciplines and most prominent in neuroscience, with single-sex studies of male animals outnumbering those of females 5.5 to 1. In the past half-century, male bias in non-human studies has increased while declining in human studies. Studies of both sexes frequently fail to analyse results by sex. Under-representation of females in animal models of disease is also commonplace, and our understanding of female biology is compromised by these deficiencies”. The study also found the justification that researchers gave for excluding female animals – that it introduced too much variability in results – to be “without foundation”. How can the current global healthcare system ever hope to rectify gender-based bias within contemporary medicine, if we are not even present at the medical trials? How are modern women supposed to navigate chronic illness and ongoing conditions, when they aren’t being considered at the baseline of experimentation?
What Does the Future Look Like?
Knowing all that we do, and feeling as deflated as ever – it’s hard to even begin to think how the issues above could be addressed, or where to start. Patriarchy, like any other system of oppression, will inevitably fall as the world becomes more knowledgeable and informed. However, for the moment, and the most part – it won’t be going anywhere just yet. We have to take pride in the small steps that are being made, and celebrate those wins, as and when they come. For all my Cysters, you’ll be happy to know that the TRAUMA of period pain is finally being recognised in medical circles. A professor of Reproductive Health at UCL (University College London), John Guillebaud revealed last year, that some period pain can be ‘as bad as having a heart attack […] men don’t get it, and it hasn’t been given the centrality it should have. I believe it’s something that should be taken care of, like anything else in medicine’. Oh, John, we’ve been waiting a lifetime to hear a similar sentiment from ANY medical professional (let alone our own – and we won’t hold our breath). In a way, it’s rewarding that finally, someone is paying attention, but I have to almost laugh at how easy John seems to think the above task is as if it’s as simple as revealing the truth that we’ve all known this entire time. How realistic is it, in a world where a woman earns 82p to the male £1; the leader of the ‘free world’ brags about grabbing women by the pussy, and female infanticide is still practised within global communities – that the rest of the world would stop and listen to women?